
































































































These Remote Towns Hold Some of America’s Most Stunning Homes
The United States offers a variety of cities and towns for almost every taste. Whether you prefer urban living with convenient amenities at your disposal, opt for being a bit removed from the busy everyday city life and move to the suburbs, or choose one of the many remote towns that dot the landscape, you have plenty of options. But there’s just something so appealing about remote living that may draw you in.
Perhaps it’s one of the many remote towns that hold some of America’s most stunning homes that you might not be able to resist, or it’s the draw of small town life with fewer crowds and less inhabitants. Or it could very well be the access to beautiful landscapes, the gorgeous nature, and the outdoor activities. Whatever your reasons for opting for remote living, there’s no denying that remote towns hold some of America’s most stunning homes.
If you're planning to relocate, opting for a second home, or simply want to look at beautiful homes in gorgeous towns, we've assembled a list of remote towns that hold some of America's most stunning homes. To determine these remote towns, Moms Who Think reviewed five-year data on median home value from the U.S. Census Bureau’s 2022 American Community Survey.
Cities, towns, and Census-designated places located at least 20 miles away from cities with populations of 50,000 or more were ranked based on median home value. Geometry attributes used to calculate the distance between city centroids came from the U.S. Census Bureau. Only remote towns with at least 500 residents were considered.
50. Kennebunkport, ME
- Median home value: $775,400
- Median household income: $113,456
- Distance to nearest city of 50,000+ residents: 21.5 miles
- Total population: 1,318
49. El Jebel, CO
- Median home value: $775,400
- Median household income: $120,278
- Distance to nearest city of 50,000+ residents: 86.6 miles
- Total population: 4,328
48. Steamboat Springs, CO
- Median home value: $776,300
- Median household income: $93,280
- Distance to nearest city of 50,000+ residents: 58.1 miles
- Total population: 13,251
47. Big Sky, MT
- Median home value: $782,100
- Median household income: $94,176
- Distance to nearest city of 50,000+ residents: 22.4 miles
- Total population: 2,825
46. Dillon, CO
- Median home value: $782,500
- Median household income: $79,792
- Distance to nearest city of 50,000+ residents: 54.9 miles
- Total population: 831
45. Tahoma, CA
- Median home value: $783,200
- Median household income: $83,971
- Distance to nearest city of 50,000+ residents: 26.4 miles
- Total population: 1,071
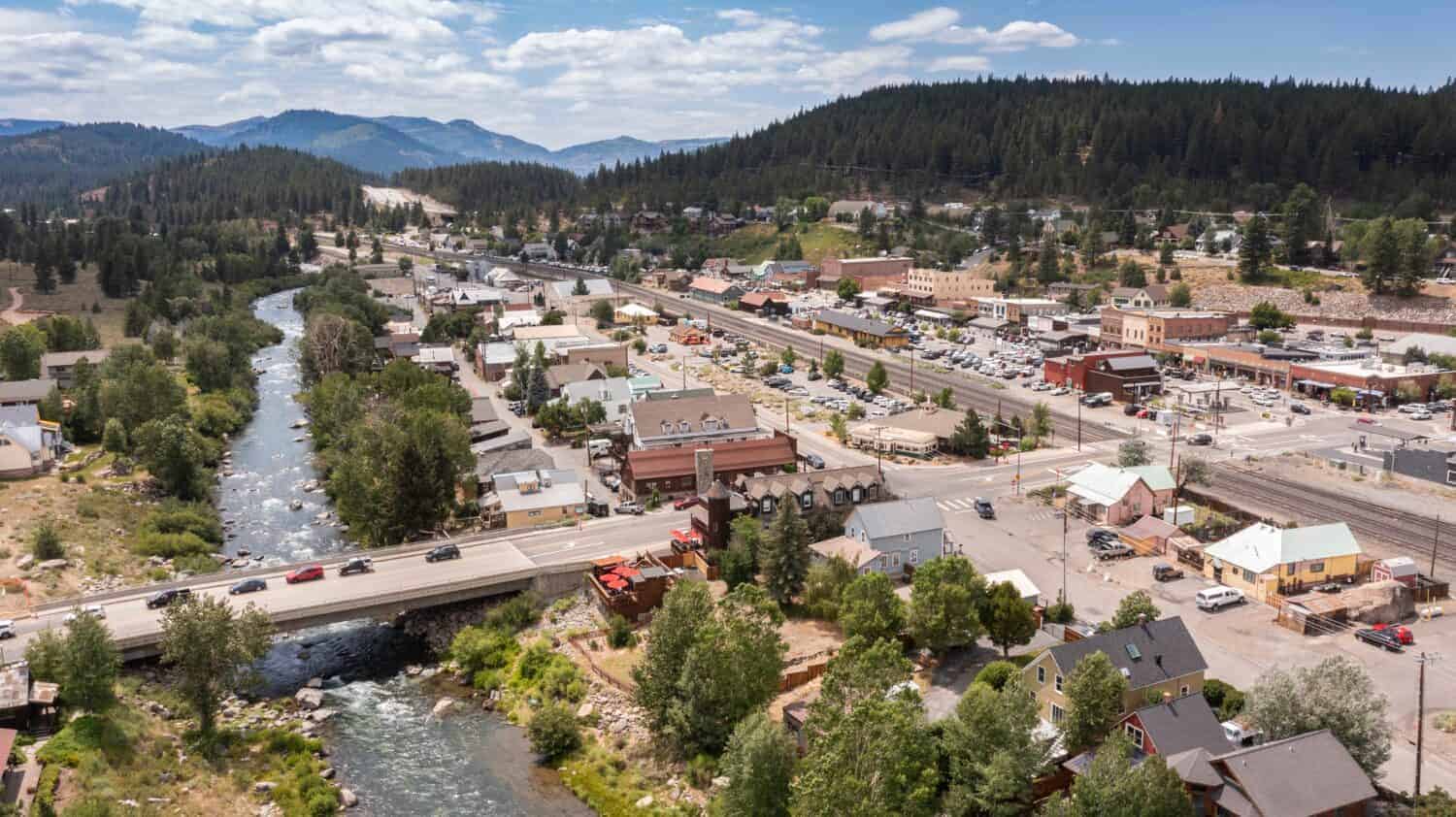
44. Truckee, CA
- Median home value: $785,700
- Median household income: $107,423
- Distance to nearest city of 50,000+ residents: 24.3 miles
- Total population: 16,784
43. Morro Bay, CA
- Median home value: $802,700
- Median household income: $88,547
- Distance to nearest city of 50,000+ residents: 33.0 miles
- Total population: 10,766
42. Key Colony Beach, FL
- Median home value: $828,800
- Median household income: $103,096
- Distance to nearest city of 50,000+ residents: 40.5 miles
- Total population: 650
41. Cambria, CA
- Median home value: $842,200
- Median household income: $95,460
- Distance to nearest city of 50,000+ residents: 49.4 miles
- Total population: 5,825
40. Aspen, CO
- Median home value: $842,700
- Median household income: $94,338
- Distance to nearest city of 50,000+ residents: 78.5 miles
- Total population: 6,952
39. Vail, CO
- Median home value: $846,600
- Median household income: $96,667
- Distance to nearest city of 50,000+ residents: 62.3 miles
- Total population: 4,833
38. Roche Harbor, WA
- Median home value: $858,100
- Median household income: $84,688
- Distance to nearest city of 50,000+ residents: 46.1 miles
- Total population: 753
37. Solvang, CA
- Median home value: $868,000
- Median household income: $108,074
- Distance to nearest city of 50,000+ residents: 24.1 miles
- Total population: 6,035
36. Groton Long Point, CT
- Median home value: $873,200
- Median household income: $118,056
- Distance to nearest city of 50,000+ residents: 24.8 miles
- Total population: 517
35. Green Harbor, MA
- Median home value: $875,600
- Median household income: $188,299
- Distance to nearest city of 50,000+ residents: 20.7 miles
- Total population: 1,174
34. Minturn, CO
- Median home value: $878,400
- Median household income: $103,333
- Distance to nearest city of 50,000+ residents: 64.3 miles
- Total population: 978
33. Mulford, CO
- Median home value: $886,400
- Median household income: $132,072
- Distance to nearest city of 50,000+ residents: 88.9 miles
- Total population: 539
32. Cedar Flat, CA
- Median home value: $900,400
- Median household income: $123,977
- Distance to nearest city of 50,000+ residents: 20.8 miles
- Total population: 948
31. Sea Isle City, NJ
- Median home value: $903,100
- Median household income: $90,703
- Distance to nearest city of 50,000+ residents: 20.0 miles
- Total population: 2,047
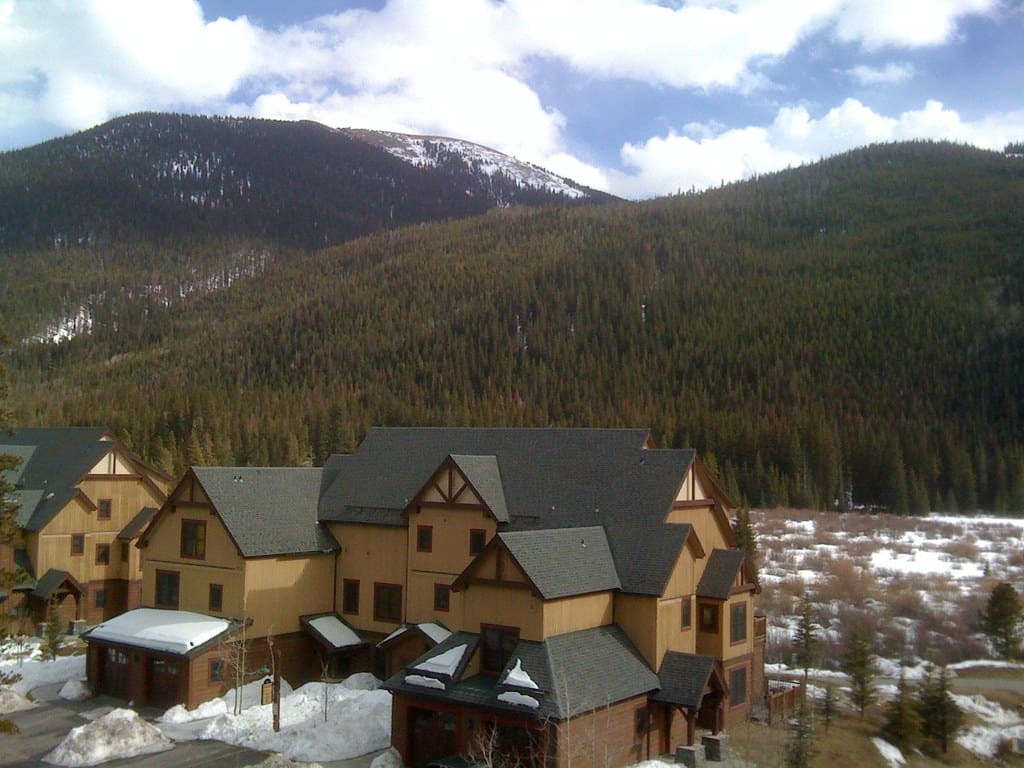
30. Breckenridge, CO
- Median home value: $903,200
- Median household income: $129,481
- Distance to nearest city of 50,000+ residents: 55.5 miles
- Total population: 5,017
29. Cayucos, CA
- Median home value: $903,700
- Median household income: $81,366
- Distance to nearest city of 50,000+ residents: 35.5 miles
- Total population: 2,361
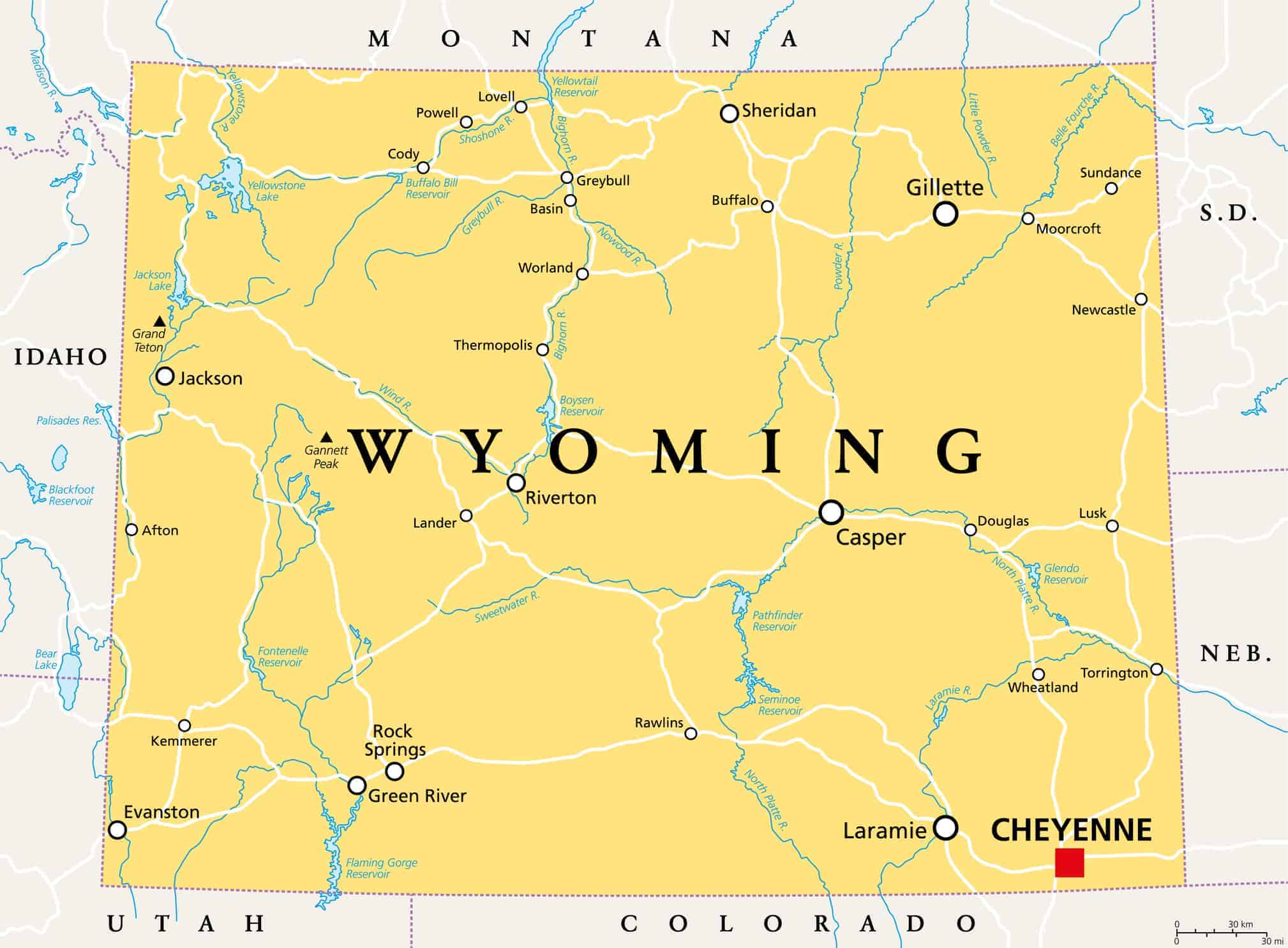
28. Rafter J Ranch, WY
- Median home value: $906,000
- Median household income: $144,844
- Distance to nearest city of 50,000+ residents: 58.5 miles
- Total population: 1,233
27. Keystone, CO
- Median home value: $910,200
- Median household income: $48,847
- Distance to nearest city of 50,000+ residents: 48.1 miles
- Total population: 995
26. Jackson, WY
- Median home value: $921,100
- Median household income: $101,477
- Distance to nearest city of 50,000+ residents: 57.9 miles
- Total population: 10,748
25. Sunnyside-Tahoe City, CA
- Median home value: $921,300
- Median household income: $125,144
- Distance to nearest city of 50,000+ residents: 25.6 miles
- Total population: 1,536
24. Sun Valley, ID
- Median home value: $921,300
- Median household income: $67,386
- Distance to nearest city of 50,000+ residents: 33.1 miles
- Total population: 1,383
23. Dollar Point, CA
- Median home value: $923,800
- Median household income: $113,269
- Distance to nearest city of 50,000+ residents: 21.8 miles
- Total population: 1,233
22. Riverpoint, WA
- Median home value: $957,200
- Median household income: $167,031
- Distance to nearest city of 50,000+ residents: 23.0 miles
- Total population: 963
21. Longport, NJ
- Median home value: $996,800
- Median household income: $101,250
- Distance to nearest city of 50,000+ residents: 22.5 miles
- Total population: 776
20. Crested Butte, CO
- Median home value: $1,013,000
- Median household income: $67,625
- Distance to nearest city of 50,000+ residents: 74.2 miles
- Total population: 1,434
19. Tres Pinos, CA
- Median home value: $1,044,500
- Median household income: $222,891
- Distance to nearest city of 50,000+ residents: 20.5 miles
- Total population: 1,006
18. Duck Key, FL
- Median home value: $1,052,700
- Median household income: $124,063
- Distance to nearest city of 50,000+ residents: 32.9 miles
- Total population: 731
17. Santa Ynez, CA
- Median home value: $1,068,300
- Median household income: $144,792
- Distance to nearest city of 50,000+ residents: 26.5 miles
- Total population: 4,716
16. DeBordieu Colony, SC
- Median home value: $1,072,800
- Median household income: $237,560
- Distance to nearest city of 50,000+ residents: 26.4 miles
- Total population: 696
15. Blue River, CO
- Median home value: $1,094,100
- Median household income: $150,074
- Distance to nearest city of 50,000+ residents: 55.2 miles
- Total population: 1,238
14. Sea Ranch, CA
- Median home value: $1,104,800
- Median household income: $92,260
- Distance to nearest city of 50,000+ residents: 52.5 miles
- Total population: 1,224
13. Basalt, CO
- Median home value: $1,106,800
- Median household income: $103,049
- Distance to nearest city of 50,000+ residents: 85.0 miles
- Total population: 3,815
12. Hoback, WY
- Median home value: $1,125,000
- Median household income: $136,436
- Distance to nearest city of 50,000+ residents: 62.4 miles
- Total population: 1,874
11. Alta, WY
- Median home value: $1,139,500
- Median household income: $161,979
- Distance to nearest city of 50,000+ residents: 47.4 miles
- Total population: 581
10. Nantucket, MA
- Median home value: $1,182,100
- Median household income: $131,736
- Distance to nearest city of 50,000+ residents: 56.0 miles
- Total population: 10,479
9. Tabernash, CO
- Median home value: $1,182,700
- Median household income: $104,335
- Distance to nearest city of 50,000+ residents: 40.9 miles
- Total population: 791
8. Avila Beach, CA
- Median home value: $1,200,300
- Median household income: $00
- Distance to nearest city of 50,000+ residents: 21.2 miles
- Total population: 1,599
7. Ballard, CA
- Median home value: $1,216,200
- Median household income: $106,458
- Distance to nearest city of 50,000+ residents: 25.3 miles
- Total population: 721
6. Los Olivos, CA
- Median home value: $1,224,400
- Median household income: $150,882
- Distance to nearest city of 50,000+ residents: 24.4 miles
- Total population: 1,020
5. South Park, WY
- Median home value: $1,283,200
- Median household income: $109,402
- Distance to nearest city of 50,000+ residents: 58.5 miles
- Total population: 1,899
4. Bodega Bay, CA
- Median home value: $1,303,000
- Median household income: $157,391
- Distance to nearest city of 50,000+ residents: 23.0 miles
- Total population: 1,186
3. Teton Village, WY
- Median home value: $2,000,000
- Median household income: $94,132
- Distance to nearest city of 50,000+ residents: 53.8 miles
- Total population: 906
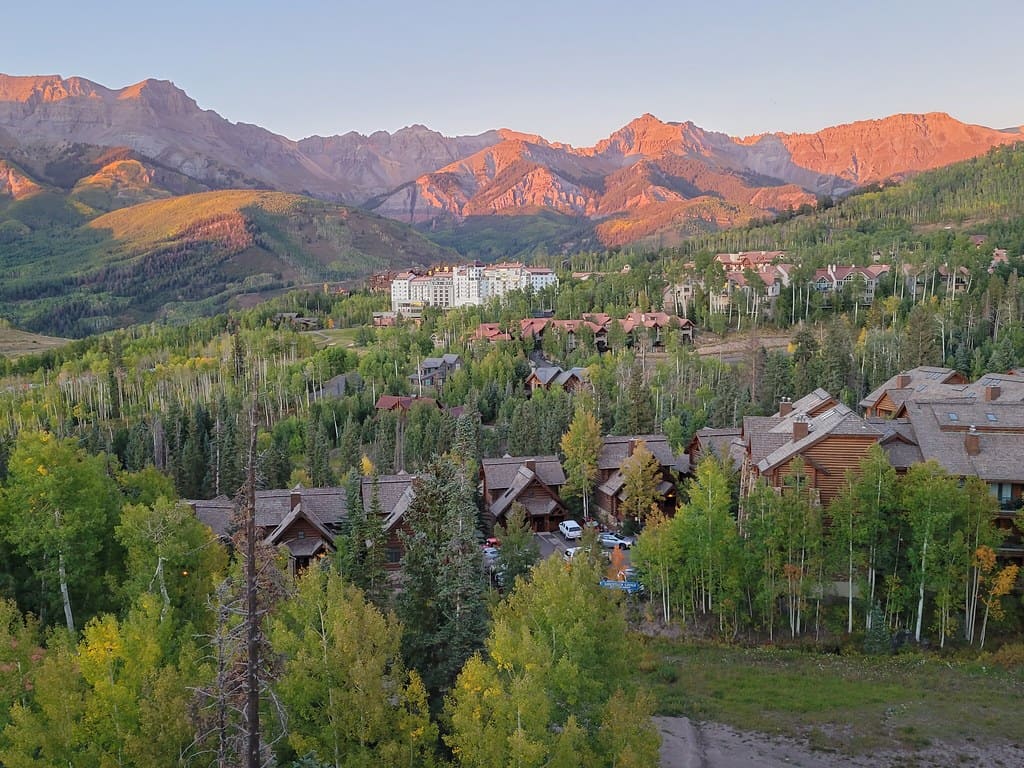
2. Mountain Village, CO
- Median home value: $2,000,000
- Median household income: $56,917
- Distance to nearest city of 50,000+ residents: 55.0 miles
- Total population: 1,582
1. Moose Wilson Road, WY
- Median home value: $2,000,000
- Median household income: $105,673
- Distance to nearest city of 50,000+ residents: 55.3 miles
- Total population: 1,143